Overactive Bladder vs. Stress Urinary Incontinence
“This information was made available with an "unrestricted educational grant from Pfizer Canada."
Overactive bladder occurs when a muscle in the bladder known as the detrusor contracts more often than normal. This causes a person to feel a sudden and sometimes overwhelming urge to urinate even when the bladder isn’t full.
The symptoms of overactive bladder include:
- Frequency — having to urinate more than 8 times over 24 hours, often including 2 or more times a night.
- Urgency — frequent, sudden, strong urges to urinate with little or no chance to postpone urination.
- Wetting accidents — (also called urge incontinence) : involuntary loss of or leaking urine following a sudden, strong desire to urinate.
- It is estimated that most people with overactive bladder experience only the symptoms of urgency and frequency (63%). The remaining 37% have wetting accidents (urge incontinence) in addition to urgency and, often, frequency.
If you have these symptoms, don’t forget one important fact – overactive bladder can be treated regardless of the cause!
Who has Overactive Bladder?
It is estimated that nearly 1 in 5 Canadians over the age of 35 suffer from overactive bladder. Overactive bladder, with frequency and urgency only, affects men and women of all ages – most people with this condition are under age 65.
Types of Urinary Incontinence
Urinary incontinence is any involuntary loss of urine even if that is not considered a problem. There are different types of incontinence whose symptoms may appear to be similar. To help avoid confusion, the different types of urinary incontinence are described below.
Urge Incontinence
Urge incontinence is a component of overactive bladder. Urge incontinence occurs when the bladder contracts involuntarily (detrusor overactivity). Symptoms include the sudden, uncontrollable need to urinate which can lead to wetting accidents. The urge to urinate can also be especially strong at night (nocturia) or may lead to accidental leakage while sleeping (enuresis).
Stress Incontinence
Stress incontinence occurs when the muscles around your urethra become too weak to prevent the urine in your bladder from escaping when the bladder pressure rises with increased abdominal pressure. Even the small amount of stress created by coughing, sneezing, laughing, exercising or lifting can result in a bit of leaking. Many women experience this after vaginal childbirth and menopause and aging, and adjust their lives by wearing pads and diapers.
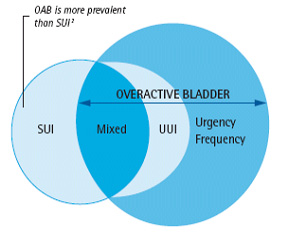
It’s important to remember that stress incontinence is NOT the same as overactive bladder. They have different symptoms, causes AND therefore, different treatments.
Mixed Symptoms (Overactive Bladder and Stress Incontinence)
Many people who have the symptoms of overactive bladder also suffer from stress incontinence. Unfortunately, there is no single treatment that works for both conditions. So if you have mixed symptoms, each will have to be treated separately.
To help you further differentiate between overactive bladder and Stress Urinary Incontinence
|
Mixed Urinary Incontinence (MUI) = Urge Urinary Incontinence (UUI) + Stress Urinary Incontinence (SUI). 3† A combination of symptoms of overactive bladder and stress incontinence is common. The most bothersome symptom (overactive bladder or stress incontinence) should be treated first.4† |
The Symptoms of overactive bladder (OAB) vs. Stress Incontinence (SI)
| Working Diagnosis – Symptoms | OB | SI |
| Urgency (strong, sudden desire to void) | Yes | No |
| Frequency with urgency (> 8 times/24 hrs) | Yes | No |
| Leaking during physical activity | No | Yes |
| Amount of urinary leakage with each episode of incontinence | Large (if present) |
Small |
| Ability to reach toilet in time following an urge to void | No | Yes |
| Waking to pass urine at night | Usually | Seldom |
References for the text:
- Abrams P. et al. The overactive bladder – A widespread and treatable condition. 1998; Erik Sparre Medical AB.
- Stewart WF, et al. Prevalence and burden of overactive bladder in the United States. World J Urol. 2003;20:327-336.
- Corcos J, et al. Prevalence of overactive bladder and incontinence in Canada. Can J Urol. 2004;77(3):2278-2284.
- Knapp PM. Identifying and treating urinary incontinence – the crucial role of the primary care physician. Postgraduate Med. 1998;103:279-294






